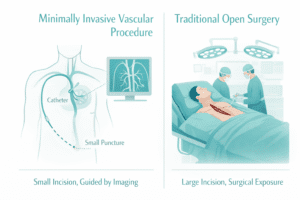
Minimally invasive vascular surgery (MIVS) has revolutionized the treatment of circulatory disorders by using advanced, catheter-based techniques rather than large incisions. These procedures allow for precise intervention on blood vessels, offering patients shorter recovery times, reduced pain, and a lower risk of complications compared to traditional open surgery.
What Is Minimally Invasive Vascular Surgery?
Minimally Invasive Vascular Surgery (MIVS) encompasses a range of endovascular procedures performed through small punctures, typically in the groin or arm. Under imaging guidance (fluoroscopy, ultrasound), interventionalists insert catheters, balloons, and stents to treat conditions such as blockages, aneurysms, and varicose veins. Common techniques include:

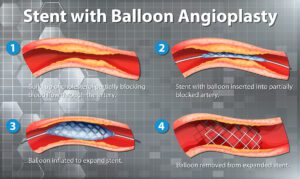
- Angioplasty and Stenting: Widening narrowed arteries with a balloon and placing a stent to keep the vessel open.
- Endovascular Aneurysm Repair (EVAR): Reinforcing weakened aortic walls with a fabric-covered stent graft to prevent rupture (source: Cleveland Clinic).
- Laser and Radiofrequency Ablation: Closing diseased veins in varicose vein treatment using thermal energy (source: Mayo Clinic).
Conditions Treated with MIVS
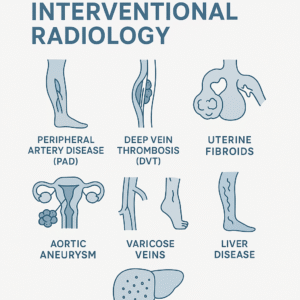
Minimally invasive methods address a broad spectrum of vascular issues:
- Peripheral Arterial Disease (PAD): Reopens arteries in the legs to restore blood flow and relieve claudication (source: American Heart Association).
- Aortic Aneurysms: EVAR offers a lifesaving alternative to open repair for abdominal and thoracic aneurysms.
- Varicose and Spider Veins: Ablation techniques deliver cosmetic improvement and symptom relief.
- Deep Vein Thrombosis (DVT): Catheter-directed thrombolysis dissolves dangerous blood clots in veins.
Benefits of Minimally Invasive Procedures
- Smaller Incisions & Scarring: Tiny punctures reduce tissue trauma and visible scars.
- Lower Infection Risk: Superficial entry points minimize exposure and postoperative infections.
- Shorter Hospital Stay: Patients often go home within one to two days versus a week or more for open surgery (source: Cleveland Clinic).
- Faster Recovery: Most resume normal activities within 1–2 weeks, compared to 6–8 weeks after open procedures.
- Reduced Pain & Blood Loss: Less disruption of muscles and organs leads to less postoperative discomfort.
- Suitability for High-Risk Patients: Those with comorbidities (heart, lung disease) tolerate endovascular approaches better than open surgery.
What to Expect: Before, During, and After
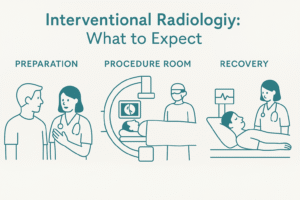
Before: Patients undergo diagnostic studies—Duplex ultrasound, CT angiography, or MR angiography—to map vessel anatomy. Pre-procedure planning includes medication adjustments and fasting instructions.
During: Under local or light sedation, the interventionalist guides catheters via small punctures. Real-time imaging ensures precise placement of balloons, stents, or grafts. Procedures typically last 1–3 hours depending on complexity.
After: Recovery begins in a monitored unit. Vital signs and puncture sites are observed. Most patients ambulate within hours and may be discharged the next day. Follow-up visits assess wound healing, vessel patency, and medication management.

Is Minimally Invasive Surgery Right for You?
Vascular specialists evaluate factors such as:
- Severity of Disease: Extent and location of arterial blockages or aneurysm size.
- Overall Health: Cardiac, pulmonary, and renal status may influence candidacy.
- Previous Treatments: History of prior surgeries or interventions.
A personalized consultation at Aria Vascular ensures an individualized treatment plan, weighing risks and benefits to achieve the best outcome.
Minimally invasive vascular surgery represents a significant advancement in circulatory care, offering effective treatment with less disruption to the body. Patients benefit from smaller incisions, quicker recoveries, and lower complication rates. If you or a loved one are experiencing vascular symptoms, schedule a consultation with Aria Vascular’s experienced team to determine if MIVS is the right option for you.